Overview of Hong Kong Cancer Statistics of 2018
1. Background
1.1 The Hong Kong Cancer Registry (HKCaR) is a population-based cancer registry responsible for collecting the basic demographic data, information of the cancer site, and cancer histology of patients diagnosed with cancer in public and private medical institutions in Hong Kong. Robust cancer registry data provide the basis for governments to prioritise resources in cancer control according to the burden of various cancers in the communities, for health care planners and researchers in developing healthcare policies to improve the quality of cancer care, prioritizing costly cancer treatments, and implementing cost-effective cancer prevention strategies such as cancer screening programmes and other public health interventions.
1.2 This is the annual overview of cancer statistics in Hong Kong that provides population-based data highlighting cancer incidence and mortality rates for 2018 and key trends for major cancers. In addition, this paper presents, for the first time, the stage-specific survival of breast and colorectal cancers.
2. New cancer cases in 2018
2.1 A total of 34,028 new cancer cases were diagnosed in Hong Kong in 2018, hitting a record high with 953 more cases or a rise of 2.9% compared to the preceding year. On average, 93 people were diagnosed with cancer each day.
2.2 Of these new cancer cases, 17,040 were diagnosed in males, and 16,988 in females. The numbers have increased by 164 (or 1.0%) for males and 789 (or 4.9%) for females compared to 2017. The crude annual incidence rates of cancer per 100,000 population were 499.7 for males and 420.4 for females in 2018.
2.3 The five most commonly diagnosed cancers in 2018 were colorectal cancer (16.6%), lung cancer (15.4%), breast cancer (13.7%), prostate cancer (6.5%) and liver cancer (5.1%), accounting for about 57% of new cancer cases diagnosed in Hong Kong in 2018. Compared with the preceding year, colorectal cancer remained stable with 5,634 cases while lung cancer increased by 1.4% to 5,252 cases and female breast cancer increased by 5.6% to 4,618 cases.
2.4 In 2018, the increase in the number of new cancer cases was mainly attributed to the growing numbers of bladder and pancreatic cancers in men, breast and corpus uteri cancers in women, as well as thyroid cancer in both genders.
2.5 For males, the top five cancers comprised about 63% of new cancer cases. They were cancers of the colorectum (19.1%), lung (19.0%), prostate (12.9%), liver (8.0%) and stomach (4.3%). They all have the number of new cases less than that in 2017.
2.6 For females, the five leading cancers were cancers of the breast (27.2%), colorectum (14.0%), lung (11.8%), corpus uteri (6.9%) and thyroid (4.7%), accounting for around 65% of new cancer cases in women.
2.7 The number of newly diagnosed invasive breast cancer in women reached over 4,600 in 2018. This marked an increase of 5.6% from 2017. In addition, 669 cases of in-situ breast cancer (i.e. stage 0 breast cancer or called pre-cancer) were diagnosed, which together recorded about 5,300 new cases of invasive and in-site breast cancer in 2018.
2.8 Cervix cancer showed a marked increase in the number of new cases compared with that of 2017, by 12.8% or 582.
2.9 The number of newly diagnosed thyroid cancer reached over 1,000 for the first time in 2018, making it the 9th most frequent cancer in Hong Kong. There was an increase of 27.6% and 14.7% in men and women, respectively. The increase was mostly accounted for by the number of micropapillary carcinoma. During the same period, there were only 50 reported deaths from thyroid cancer, indicating an overall good prognosis of this cancer.
2.10 Compared to 2017, there was an increase of 11.6% in the number of newly diagnosed pancreatic cancer, up to a total number of 855 cases. The number has increased by 91% since 2008. Although pancreatic cancer only being the 11th most common cancers, it was the 5th leading cause of cancer deaths in Hong Kong with 711 deaths recorded in 2018, indicating an overall poor prognosis of this cancer.
2.11 Compared to a decade earlier, new cancer cases have jumped by about 38% or at an annual rate of 3.3%. During the same period, the population grew slowly at an annual rate of 0.7%, but the population aged 65 and older increased at 3.7% per year.
2.12 As cancer incidence rates increase sharply with age, the increase in overall cancer incidence rate in Hong Kong is largely driven by an ageing and growing population, along with changes in cancer risks as well as the improvements in diagnostic practices.
2.13 The type and order of five leading cancers have remained more or less the same over the years (Table 1). The biggest increases over the past decade were in colorectal cancer among men and breast cancer in women, with about 44% and 77% inclinations in the number of new cases, respectively. The annual number of new cases of liver cancer has remained stable in recent years.
Table 1. Leading cancer types (both genders combined)
Rank in
2018 Cancer type No. of new cases
in 2008 (rank) No. of new
cases in 2018 Overall
change
All cancers 24,635 34,028 +38.1%
1 Colorectum 4,031 (2) 5,634 +39.8%
2 Lung 4,236 (1) 5,252 +24.0%
3 Breast 2,633 (3) 4,645 +76.4%
4 Prostate 1,369 (5) 2,204 +61.0%
5 Liver 1,745 (4) 1,742 -0.2%
3. Cancer deaths registered in 2018:
3.1 Cancer was the number one killer in Hong Kong in 2018 with 14,594 cancer deaths, accounting for 30.7% of all deaths in Hong Kong. Over half (58%) of the cancer deaths were in men. The crude annual mortality rates of cancer per 100,000 population were 250.0 for males and 150.2 for females in 2018.
3.2 The top three causes of cancer deaths were lung cancer (26.4%), colorectal cancer (15.9%) and liver cancer (10.2%), which accounted for over half of all cancer deaths.
3.3 For males, cancers of the lung (29.6%), colorectum (15.4%) and liver (12.8%) accounted for nearly 60% of the cancer deaths.
3.4 The cancers causing most deaths in females were lung cancer (21.9%), colorectal cancer (16.6%) and breast cancer (12.4%), accounting for nearly half of all cancer deaths.
3.5 Over the past decade, the number of cancer deaths has risen at an annual rate of 1.6% per year. The ranking of top five deadliest cancers almost unchanged (Table 2). There were marked increases in the number of deaths from pancreatic cancer (66.9%) and breast cancer (46.8%). The increase was much less pronounced in lung cancer (10.2%).
Table 2. Leading cancer deaths (both genders combined)
Rank in
2018 Cancer type No. of deaths in
2008 (rank) No. of deaths in
2018 Overall
change
All cancers 12,456 14,594 +17.2%
1 Lung 3,497 (1) 3,853 +10.2%
2 Colorectum 1,686 (2) 2,314 +37.2%
3 Liver 1,499 (3) 1,487 -0.8%
4 Breast 515 (5) 756 +46.8%
5 Pancreas 426 (6) 711 +66.9%
3.6 The increase in the number of new cancer cases and cancer deaths was primarily attributed to an ageing and growing population. As long as the current demographic trends continue in Hong Kong, we shall be witnessing an elevated incidence and mortality burden of cancer in the population.
Appendix 1 displays the ten cancers with the largest number of new cases diagnosed and cancer deaths by gender in 2018.
4. Cancer and gender
4.1 More men developed cancer than women but the difference narrowed to 52 cases in 2018. With the prevailing trends in incidence and population structure, it is expected that females will suppress males in the number of cancer cases in the next few years.
4.2 The cancers with the highest male to female ratio were cancers of the larynx (male to female ratio=14.7:1), oesophagus (4.5:1) and liver (3.5:1).
4.3 The only two cancers that were more common in women than men were thyroid cancer (female to male ratio=3.5:1), and breast cancer which just a mere 0.6% developed in men.
4.4 More men died from cancer (8,526) than women (6,068), with a male to female ratio of 1.4 to 1.
5. Cancer and age
5.1 Cancer is primarily a disease of older people. Half of cancers occurred in people over the age of 65, whereas only a mere 0.6% of cancers being diagnosed in children and adolescents (i.e. aged 0-19 years).
5.2 Women are more prone to have cancer than men among adults between the ages of 20 and 59 years, mainly due to the relatively high incidence rates of gender-specific cancers of the breast, cervix, corpus uteri and ovary. The age-specific female preponderance was most apparent in the age group of 20-44 years, in which the number of cancers in women was more than twice of that in men.
5.3 The median age of patients at diagnosis of cancer in 2018 was 68 years in men and 62 years in women while the median age of cancer deaths in 2018 was 72 years in both men and women.
5.4 Among the common cancers in males, the median age at diagnosis was 68 years for colorectal cancer, 70 years for lung cancer, 71 years for prostate cancer, 65 years for liver cancer, and 70 years for stomach cancer.
5.5 Among the common cancers in females, the median age at diagnosis was 57 years for breast cancer, 68 years for colorectal cancer, 68 years for lung cancer, 55 years for cancer of the corpus uteri, and 50 years for thyroid cancer.
5.6 There were 189 newly diagnosed cancer cases in children and adolescents in 2018, 92 in males and 97 in females. The more common children and adolescent cancers were leukaemia (33.3%), lymphoma (15.9%) and germ-cell and gonadal tumours (12.2%). The top three cancers constituted about 61% of all cancers in children and adolescents.
5.7 In young adults aged 20-44 years, the most common cancer was nasopharyngeal cancer for males and breast cancer for females. Colorectal cancer retained second place in men.
5.8 In adults aged 45-64 years, the most common cancer was colorectal cancer for males and breast cancer for females.
5.9 In elderly people aged 65-74 years, lung cancer moved past colorectal cancer to become the most common cancer for males again. The most common cancer was breast cancer for females.
5.10 In very elderly people aged 75 or older, the most common cancer was lung cancer for males and colorectal cancer for females.
5.11 A person’s risk of developing or dying from cancer is age-dependent. Based on the cancer statistics collected in 2018, about 1 in 4 men and 1 in 5 women will develop cancer before the age of 75. About 1 in 9 men and 1 in 15 women will die from cancer before the age of 75.
Appendix 2 displays the relative frequency of the five most common cancers by gender and age groups in 2018.
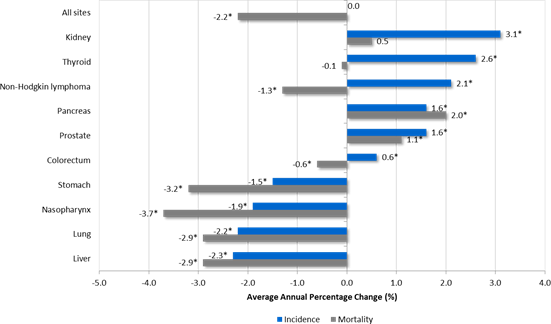
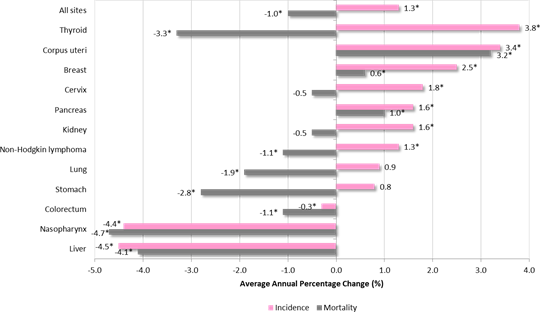
6. Trends in incidence and mortality in the last decade, 2009-2018
6.1 Age-standardised rate (ASR) is a statistical measure of the risk of cancer after accounting for the influence of age, which is widely used to measure trends over time or between two different populations. Average Annual Percent Change (AAPC) of ASR was estimated using cancer registry data from 1991-2018 to summarize the trends over the 10-year period from 2009 to 2018. A p-value of less than 0.05 (p<0.05) was considered statistically significant.
6.2 In the period from 2009 to 2018, the overall age-standardised incidence rate (ASI) for all cancers in males seemed to be levelling off after the decline in the past two decades, while a significant trend of increasing ASI in females was observed at an annual rate of 1.3% (p<0.05) in the same period.
6.3 The age-standardised mortality rates (ASM) were decreasing for both genders, at -2.2% per year (p<0.05) among males and -1.0% per year among females (p<0.05) in that period.
6.4 Among the common cancers, a significant trend of decreasing incidence (ASI) was most apparent in cancers of the nasopharynx (AAPC: -1.9% in males; -4.4% in females) and liver (AAPC: -2.3% in males; -4.5% in females) in both genders, as well as stomach (AAPC: -1.5%) and lung (AAPC: -2.2%) in males (Figures 1 and 2).
Figure 1. Average annual percent change (AAPC)1 of age-standardised rates2 of common cancers over the period 2009-2018, Males
Figure 2. Average annual percent change (AAPC)1 of age-standardised rates2 of common cancers over the period 2009-2018, Females
Notes:
1. Average Annual Percent Change (AAPC) of age-standardised rates over the past ten years is estimated from joinpoint regression (Reference: Clegg LX, Hankey BF, Tiwari R, Feuer EJ, Edwards BK. Estimating average annual percent change in trend analysis. Statistics in Medicine 2009; 28(29): 3670-82.), based on the available data from 1991 to 2018. An asterisk (*) represents the AAPC is statistically significant from zero at 5% level (p<0.05).
2. Rates are age-adjusted to the age distribution of the World Standard Population of Segi (1960).
6.5 A significant trend of rising incidence (ASI) was observed for cancers of the thyroid (AAPC:
+2.6% in males; +3.8% in females), kidney (AAPC: +3.1% in males; +1.6% in females), pancreas (AAPC: +1.6% in males; +1.6% in females) and non-Hodgkin lymphoma (AAPC: +2.1% in males;
+1.3% in females) in both genders, breast (AAPC: +2.5%), cervix (AAPC: +1.8%) and corpus uteri (AAPC: +3.4%) in females, as well as the prostate (AAPC: +1.6%) and colorectum (AAPC: +0.6%) in males.
6.6 In terms of mortality (ASM), a significant decreasing trend was observed in most cancers, with the exception of pancreatic cancer (AAPC: +2.0% in males; +1.0% in females) in both genders, prostate cancer (AAPC: +1.1%) in males and cancers of the breast (AAPC: +0.6%) and corpus uteri (AAPC: +3.2%) in females. No significant changes were observed in cancer of the cervix in females.
7. Special issue – First report of stage-specific survival of breast and colorectal cancers in Hong Kong
7.1 Cancer stage is an important prognostic information for people diagnosed with cancer. As such, the HKCaR has made considerable efforts to improve the collection of staging data for prevalent cancers in recent years.
7.2 As the quality and completeness of the breast cancer (BRC) and colorectal cancer (CRC) staging data are high enough for robust analysis of survival by stage at population level, the HKCaR compiles and presents, for the first time, a report of stage-specific survival of breast and colorectal cancers in Hong Kong, and will continue to do so moving forward to include more prevalent cancers.
7.3 Based on the analysis of survival involving more than 66,000 BRC and CRC patients diagnosed in 2010-2017 with follow-up to 2019, the overall 5-year relative survival rates (RSR) of BRC and CRC were 84.0% and 58.2%, respectively.
7.4 In other words, compared to a group of similar individuals in the general population who do not have BRC, 84.0% of BRC patients would survive 5 years or more after diagnosis. The 5-year RSR was 99.3% for stage I, 94.6% for stage II, 76.2% for stage III and 29.8% for stage IV.
7.5 The overall 5-year relative survival rate of colorectal cancer was 58.2%. The 5-year relative survival rates were high for stage I (95.7%) and stage II (87.3%). It dropped to 68.7% for stage III and further declined to 9.3% for stage IV.
Key Messages
New cancer cases jumped by about 3% in a year, reaching a record high of 34,028 in 2018. On average, 93 people were diagnosed with cancer each day.
The ratio between the number of new cases in men and women has narrowed over time, where men outnumbered women by just 52 cases in 2018.
Colorectal cancer remained the most common cancer in men, while breast cancer was still the leading cancer in women.
In men, both the number of new colorectal and prostate cancer cases remained consistently high, despite no further increase being observed in 2018.
In women, the number of new breast cancer cases was still on the rise, with a surge of 5.6% in 2018 and a rise of 77% over ten years, the biggest rise in number among the top 5 cancers.
Stage I breast cancer had a 5-year relative survival rate of 99%, which means that these individuals were almost as likely to survive (more than 5 years) as women without the disease in the population. Stage IV breast cancer had a 5-year relative survival rate of 30%.
For colorectal cancer, the overall 5-year relative survival rate was 58%. The rates were high for stage I (96%) and stage II (87%). It was 69% for stage III but declined to 9.3% for stage IV.
Age-standardised cancer incidence rates for men seemed to be leveled off, with an increasing trend for women observed in the past decade. Both age-standardised mortality rates for men and women had a downward trend during the same period.
Age-standardised incidence rates have increased over the past decade in the following cancer sites, indicating the increasing numbers of these cancers in the local population could only be partially attributable to the aging population:
– Male: prostate, colorectum, non-Hodgkin lymphoma and pancreas
– Female: breast, cervix, corpus, non-Hodgkin lymphoma, pancreas and thyroid
Dr. K.H. Wong
Director, Hong Kong Cancer Registry Hospital Authority
21 October 2020
Appendix 1: Leading Cancer Sites in 2018
* All rates are expressed per 100,000 population. Rates for gender-specific sites are per 100,000 male or female population. Statistics on the number of deaths are provided by the Census and Statistics Department and Department of Health of HKSAR.
Appendix 2: Five Most Common Cancers by Gender and Age Group in 2018
* The classification of cancers in children and adolescents (0-19 years) is based on the morphology according to the “International Classification for Childhood Cancer 1996, IARC Technical Report No. 29: Lyon, 1996.”, rather than the site of tumour.
Note on the use of data:
The numbers of new cases and deaths are important parameters to measure the burden of cancer on local healthcare system. One should keep in mind that the figures are subject to random fluctuations from year to year. Experience tells us that a more reliable comment on the trends of incidence and mortality can only be made after observing over a longer period of preferably at least 5 years or more.
Suggested citation:
Hong Kong Cancer Registry. Overview of Hong Kong Cancer Statistics of 2018. Hong Kong Hospital Authority; Oct 2020. Available at: https://www3.ha.org.hk/cancereg (accessed [date]).
More cancer statistics are available on the website of Hong Kong Cancer Registry: https://www3.ha.org.hk/cancereg